Matthew Manz, BScPharm A practical approach to opioid use disorder patient care in Ontario: a pharmacist’s perspective
Jana Mayer, BScPhm, RPh Pharmacists and prescribers: exploring the potential for complementary, synergistic roles in fighting the opioid crisis
Ajit Johal, RPh, BSP, BCPP, CTH Toward integrated care and improved access to pharmacotherapy for patients with opioid use disorder: an addiction medicine physician’s perspective
Feng Chang, PharmD Access to care – a BC perspective: how pharmacists can be supported in helping OUD patients overcome barriers to care
Lisa Lefebvre, MDCM, MPH, FCFP(AM), DABAM, CCSAM, FASAM, CMRO

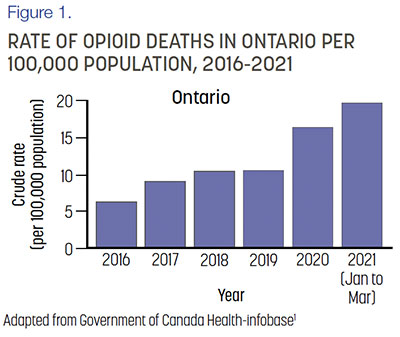
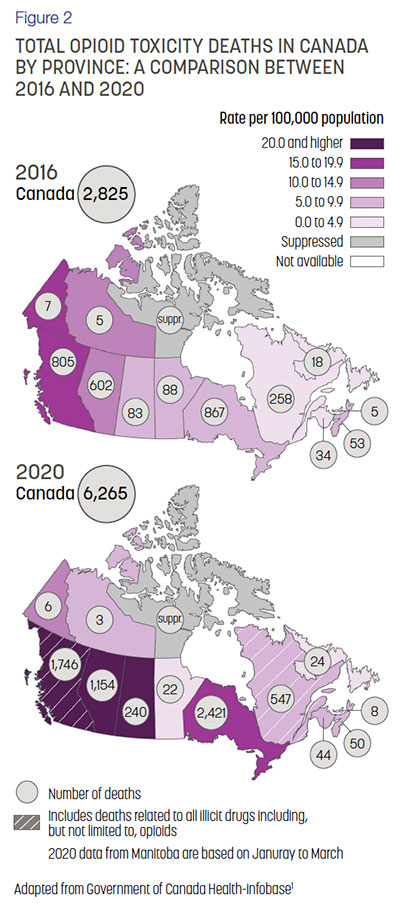
Opioid-related deaths in Ontario have doubled since 2017, with significant increases since the COVID-19 pandemic in 2020 (Fig. 1).1 This trend is also seen in Canada as a whole (Fig. 2). There is a clear need for a better practical approach in opioid care in Ontario and Canada alike. While the opioid crisis is clearly multi-faceted, and no simple solution exists, I believe that improving access and enlightening resources to patient care in Ontario is one of the most important parts of fighting the opioid crisis. Just as pharmacists were able to contribute to improving the COVID-19 crisis by administering the vaccine, we may be able to contribute to improving the opioid crisis by offering collaborative patient care.
Pharmacists play a key role as accessible, visible healthcare providers who have the skills and knowledge to offer hands-on care to opioid use disorder (OUD) patients. As a pharmacist in Toronto, Ontario, I am keenly aware of the opioid crisis, and I offer a variety of care and treatment options to my patients with OUD.
Currently, there are significant barriers and misconceptions preventing pharmacists from offering complete practical care to opioid users. I will outline these barriers and my clinic’s method for navigating the current regulations. Finally, I propose changes that could help engage pharmacists in providing treatment, and ultimately help resolve the opioid crisis in Ontario.
Regulatory barriers for pharmacists in Ontario
Currently, it is a challenge for pharmacists to offer opioid agonist therapy (OAT) to patients who want to stop using prescription or illicit opioids. This is partly due to limited health care practitioner availability due to the COVID-19 pandemic. As far as I am aware, I was the first pharmacist in Ontario to regularly administer long-acting injectable therapies to patients who were not able to find a regulated health care provider to inject OAT because of the shift toward virtual care appointments.
In order to dispense methadone and buprenorphine, Ontario pharmacists must complete a training course within 6 months of starting to provide OAT to their patients.2 Training is also recommended for pharmacists to understand structured treatment and to be vigilant in observing doses. In order to have access to extended-release buprenorphine, pharmacists and prescribers must complete subcutaneous injection training and attend online courses for clinical knowledge, offered by the manufacturer of the injectable medication.
In order to administer long-acting extended-release buprenorphine by injection, pharmacists legally require the sign-off of a medical directive from a prescribing physician or other regulated healthcare professional to perform this delegated task. Long-acting extended-release injectable buprenorphine is available to order by pharmacists through a controlled distribution process via the manufacturing warehouse, not from our regular wholesaler. This medication can’t be dispensed directly to the patient to take to the physician office to inject due to the required chain of signatures as well as the need to be refrigerated.
The requirement of a medical directive in Ontario creates an extra step and it may discourage pharmacists who are otherwise willing and able to offer such a service. An extended scope of practice for pharmacists could remove this barrier, making it easier for pharmacists to offer these services instead of the medication having to be delivered from the pharmacy to the physician’s office for injection. In most provinces like Alberta and Manitoba, a medical directive is not required to inject OAT.
There has been some headway in reducing the barriers to prescribers. Since 2018, physicians no longer require an exemption to prescribe methadone, buprenorphine or other OAT treatment. It is my hope that similar progress will be made in reducing the barriers mentioned above for pharmacists in Ontario to do the same in the near future.
Background on treatments for opioid use disorder
Both methadone and buprenorphine are long-acting medications that bind to opioid receptors in the brain, quelling cravings without causing a person to feel euphoria.5 Methadone is a medication with a long history of use, and it is administered orally. Buprenorphine is a newer medication which can be administered sublingually, buccally, via subcutaneous injection, via a transdermal patch6 or subdermal implant.7 Both medications are effective as treatment for opioid use disorder, and with diligent use of the therapy, some patients are able to stop using illicit opioids without having to go through withdrawal symptoms.8
Opioid agonist therapy must be prescribed and dispensed by a healthcare professional along with ongoing life counseling to manage addiction. Offering these valuable resources can prevent and explain patterns that lead to triggers which may cause the individual to relapse. Many factors, including culture, gender, financial situation and family can all impact how patients do in treatment. Pharmacists provide support through daily interactions and can advocate for positive changes in their patients’ lives.
The Canadian Research Initiative in Substance Misuse (CRISM) National Opioid Use Disorder Guideline recommends buprenorphine / naloxone formulations as a first-line treatment option for OUD because of its superior safety profile when compared to methadone.9
In terms of method of administration, both oral options and long-acting injectable medications have their benefits. The oral medication is easier for healthcare providers to dispense and observe. The daily routine of coming into the clinic or pharmacy for treatment can also contribute to the patient’s psychosocial recovery process. Over time, their doctor may decide that they are eligible for take-home “carry doses” for self-administration, once patients are stable and understand the process to recovery. With carry doses there is a risk of misuse and diversion of these medications into the community, although some formulations, such as buprenorphine, are combined with naloxone to reduce this risk.10 Diversion and inappropriate use may result in overdoses among adolescents, adults and accidental ingestion causing death in children.
Long-acting injectable buprenorphine formulations form a very small mass under the skin which provides a constant blood level of medication over time.11 This may provide a more consistent dose. Patients may benefit from not having to come into the clinic or pharmacy as often, which is helpful if they live far away from their nearest OAT pharmacy or have jobs with long hours.12 The clinician benefits from less foot traffic in the clinic or pharmacy and fewer demands on their time. However, the subcutaneous injections can be more logistically challenging to administer than a simple oral medication dosing, and may also require special training, an ordering platform, and examination tables for patients to lay down during injection administration.
Working effectively within Ontario’s regulations
Despite the significant barriers to pharmacists in providing OAT, my pharmacy has developed an effective method and network for providing this therapy under the current regulations.
The most important aspect of our approach is to facilitate excellent collaboration between physicians and pharmacists. My pharmacy is set up to connect with trueNorth medical centers and physicians, a service providing comprehensive addiction medicine to individuals within Ontario who are facing substance use challenges. We use a secure text-based platform where we can send messages and urine drug screening (UDS) results between our clinic and the physician’s office. This allows us to monitor the patient’s progress and guide them through the long journey to recovery. Good networking and collaboration between the pharmacist and physician is very helpful, and should become standard practice in addiction medicine.
Alongside trueNorth physicians, my pharmacy has also developed a proprietary documentation log system to record all injections and comply with regulations. In addition, we have a standardized medical directive that physicians can fill out, requesting that our pharmacists administer buprenorphine injections. The steps we have developed enables us to more easily provide effective care. I believe a standardized system and a reimbursement fee for the injection service would help pharmacists to step in and offer this care. In the next section, I will outline the changes I think would help facilitate the provision of care by pharmacists.
Future directions: how to engage and support pharmacists
Pharmacists currently face challenges in providing effective care, including OAT, to people who struggle with opioids and are overdosing frequently. Here, I will discuss the importance of pharmacists’ role in providing practical OAT, and propose solutions that would engage and support pharmacists in offering this kind of care.
Most people are able to access a pharmacist for a medication refill, advice or just simple help, every day of the week, in their immediate neighborhood. Physicians who are specialized in addiction medicine, however, may be located a considerable distance from a patient’s home. Injectable buprenorphine is a beneficial treatment option that may not be available to many patients right now who wish to receive it and instead they have to use methadone or sublingual buprenorphine daily. Pharmacists are the missing piece in connecting patients to the sustainable treatments that they need.
Pharmacists may be encouraged to offer injectable OAT if some of the barriers were removed. I suggest that changes to the pharmacist’s scope of practice and reimbursement for the provision of care could potentially reduce the amount of time involved. The province of Alberta and Saskatchewan, for example, allows pharmacists to administer injections to patients if they complete an additional certification.13 This ensures compliance with all legal and safety measures that may be also provided to Ontario pharmacists.
The majority of buprenorphine injections are given by doctors or nurses at their clinics, but this creates a significant strain on the doctor’s time and right now many are working entirely virtually. Pharmacists are capable, available, and accessible healthcare providers who can take on this responsibility. Unlocking this large group of providers would help improve or maybe resolve the opioid crisis. While these changes would be major, they are not unprecedented.
Reducing these barriers with the solutions proposed here could help engage more pharmacists in providing different kinds of OAT to patients.
Conclusion
Ontario is in an opioid crisis made worse by a global pandemic and economic crisis. Currently, we need all pharmacists who can step in to support other healthcare providers in providing compassionate care to this population to fight opioid addiction.
By connecting patients with addiction prescribers and utilizing many resources, we are able to provide a practical approach to OUD patients. At my pharmacy we are making a difference one patient at a time. It is my hope that my pharmacy’s practices and the suggestions I have outlined here will inspire other pharmacies to get involved and help provide safe, effective treatment for OUD patients. Together, pharmacists have a lot of potential to make a difference.
ACKNOWLEDGEMENTS
Editorial Assistance. Editorial assistance was provided by Laura Tennant, HBSc (Toronto, Canada), and STA Healthcare Communications (Montreal, Canada). Support for this assistance was funded by Indivior Canada.
Disclosures. Jana Mayer has received honorarium from Indivior for 2 presentations. She has not received any honorarium for the article.
References
1. Opioid- and Stimulant-related Harms in Canada. Accessed October 28, 2021. https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants/
2. Opioid Use Disorder Treatment for Pharmacists: Ontario – OCPInfo.com. Accessed October 28, 2021. https://www.ocpinfo.com/education_resource/opioidusedisordertreatmentforpharmacistsontario/
3. Kalvik A. Buprenorphine for the Treatment of Opioid Dependence. Pharmacy Connection (Winter 2014):21-31.
4. Administering a Substance by Injection or Inhalation – OCPInfo.com. Accessed October 29, 2021. https://www.ocpinfo.com/regulations-standards/practice-policies-guidelines/inhalation/
5. Connery HS. Medication-Assisted Treatment of Opioid Use Disorder: Review of the Evidence and Future Directions. Harv Rev Psychiatry. 2015;23(2):63-75. doi:10.1097/HRP.0000000000000075
6. Government of Canada HC. Drug Product Database Online Query. Published April 25, 2012. Accessed November 10, 2021. https://health-products.canada.ca/dpd-bdpp/info.do?lang=en&code=82676
7. Government of Canada HC. Drug Product Database Online Query. Published April 25, 2012. Accessed November 10, 2021. https://health-products.canada.ca/dpd-bdpp/info.do?lang=en&code=96515
8. Connock M, Juarez-Garcia A, Jowett S, et al. Methadone and Buprenorphine for the Management of Opioid Dependence: A Systematic Review and Economic Evaluation. NIHR Journals Library; 2007. Accessed October 28, 2021. https://www.ncbi.nlm.nih.gov/books/NBK62286/
9. Bruneau J, Ahamad K, Goyer M-È, et al. Management of opioid use disorders: a national clinical practice guideline. CMAJ. 2018;190(9):E247-E257. doi:10.1503/cmaj.170958
10. Blazes CK, Morrow JD. Reconsidering the Usefulness of Adding Naloxone to Buprenorphine. Front Psychiatry. 2020;11:958. doi:10.3389/fpsyt.2020.549272
11. Ling W, Shoptaw S, Goodman-Meza D. Depot Buprenorphine Injection In The Management Of Opioid Use Disorder: From Development To Implementation. Subst Abuse Rehabil. 2019;10:69-78. doi:10.2147/SAR.S155843
12. Eibl JK, Gauthier G, Pellegrini D, et al. The effectiveness of telemedicine-delivered opioid agonist therapy in a supervised clinical setting. Drug Alcohol Depend. 2017;176:133-138. doi:10.1016/j.drugalcdep.2017.01.048
13. Saskatchewan College of Pharmacy Professionals. Prof Practice - Administration of Drugs by Injection... - Saskatchewan College of Pharmacy Professionals. Published 2021. Accessed October 17, 2021. https://saskpharm.ca/site/profprac/adminofdrugs?nav=sidebar